Washington State Builds a Stronger Mental Health Workforce: Introducing the Bachelor's Level BHSS (Webinar August 28)
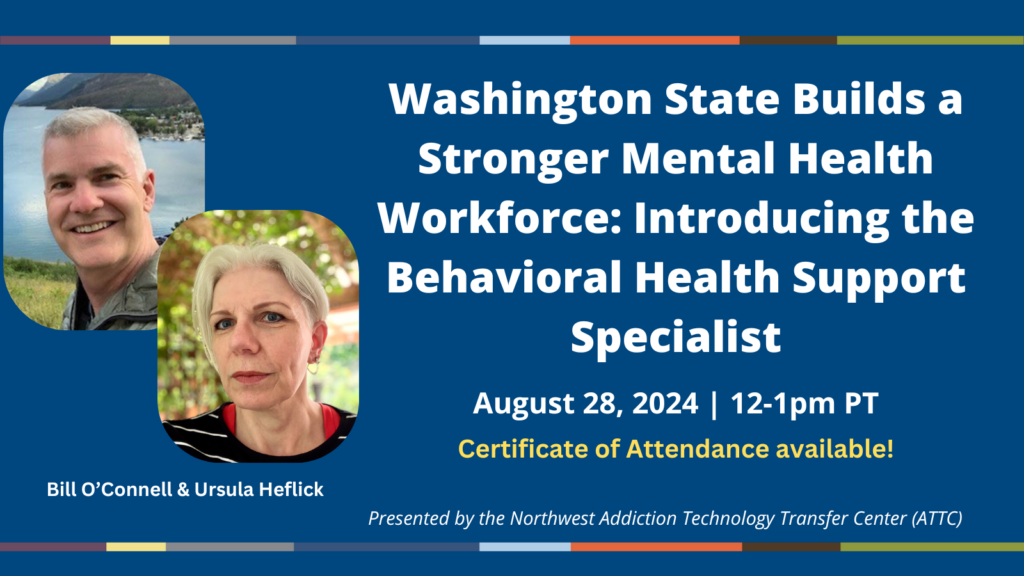
Join the Northwest ATTC and speakers Bill O'Connell, EdD (UW Psychiatry) and Ursula Heflick (Spokane Fall Community College) for a webinar on August 28, 2024 (12-1pm PT) about an innovative new effort in Washington State to initiate a bachelor's-level Behavioral Health Support Specialist (BHSS) curriculum leading to credentialing to expand the mental health workforce and improve access to care.
The mental and behavioral health workforce shortage has hindered access to care in the United States, resulting in long waitlists for persons who need behavioral health care. Bachelor level practitioners are one solution to increasing available mental and behavioral health treatment across a variety of settings. A Behavioral Health Support Specialist (BHSS) will provide brief treatment for depression using behavioral activation, anxiety using CBT and engage in harm reduction for substance use issues.
This webinar will describe the relationship between approved bachelor programs in behavioral health, psychology, and social work and the new state BHSS credential and help participants understand the role and function of the BHSS in the various settings they can practice under supervision.
A certificate of attendance (for CE credits) will be sent to all attendees of the live webinar.