
Introduction
Over the past decade, the abuse of prescription and illegal opioids rapidly evolved to become one of the most significant public health challenges in the United States today. This challenge is felt keenly in rural and frontier communities. Rural communities struggle with the largest increases in opioid related morbidity and mortality and the most limited access to treatment options. The National Rural Health Association’s (NRHA) recent brief, Treating the Rural Opioid Epidemic, summarizes the nature of this challenge and identifies policy recommendations for increasing access to Medication-Assisted Treatment (MAT) and other needed recovery supports in rural communities.
Moving policy recommendations from paper to implementation is a daunting task. Too often, such recommendations are ineffectively implemented and wither before people in need can benefit from them. Opioid abuse is a pervasive problem crossing complex and siloed systems, including criminal justice, health and mental health, and child welfare; creating change in complex systems is challenging when states and communities have limited resources, readiness, and capacity. As states and communities consider the NRHA recommendations and how best to respond to the rural opioid epidemic, Implementation Science can offer insight into how to ensure these recommendations can be embedded and sustained so that rural communities can benefit.
Rural Implementation Formula
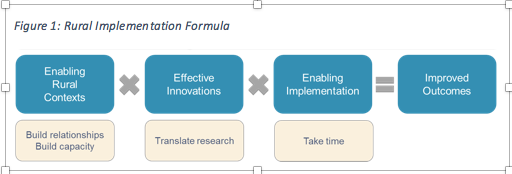
Implementation Science is the study of how programs based in research evidence can be best implemented and sustained in communities and systems. Research on implementation of health and human services programs demonstrates that effective implementation requires not just evidence-based programs, such as those identified in the NRHA recommendations, but three implementation components (NIRN):
Our work at the National Implementation Research Network (NIRN) in rural and frontier communities has found that these three components are difficult to build and sustain in rural communities.
Based on our experience, we believe that rural communities require a different approach to implementing policy and practices – an approach that begins with building enabling context, and then translates research evidence so that it is relevant to the context. Without approaching rural implementation differently, we believe that disparities between rural and urban or suburban communities will increase. Currently, rural communities are less likely to implement evidence-based programs than urban or suburban peers (Dotson et al., 2008). Our work suggests that this disparity is because evidence-based and evidence-informed programs are more likely to be successfully implemented by communities with higher capacity and greater financial and workforce resources. Developing strategies to address this inequity is essential to meeting the needs of rural communities and reducing rural disparities. Our Rural Implementation Formula provides a guiding strategy for funders, researchers, practitioners and community members seeking to apply the best of Implementation Science to implement the NRHA recommendations in their work.
Enabling Rural Context
Successfully treating the opioid crisis requires connecting effective policy at the state and federal level to the realities of rural opioid 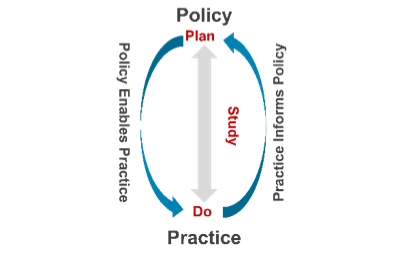 addiction. Funders and government agencies must develop and support a Practice-Policy Feedback Loop between rural communities and the other systems that fund, train and monitor them. This represents a radical shift in the traditional dynamic between rural communities and those in positions of power. Typically, rural communities have decisions made for them: funders and state agencies determine what strategies will be implemented before rural communities have an opportunity to fully consider their own needs and evaluate options. These traditional dynamics result in a status quo that does not shift to accommodate new programs or practices; instead, new programs and practices are changed to fit the system (Metz & Bartley, 2012). In order for policy to effectively enable practice in communities, it must be informed by practice. When policy-practice feedback loops are institutionalized within a system, they can promote systems change. Formal, transparent and ongoing bi-directional communication between rural communities and state and federal partners can help push the NRHA recommendations from paper to practice.
addiction. Funders and government agencies must develop and support a Practice-Policy Feedback Loop between rural communities and the other systems that fund, train and monitor them. This represents a radical shift in the traditional dynamic between rural communities and those in positions of power. Typically, rural communities have decisions made for them: funders and state agencies determine what strategies will be implemented before rural communities have an opportunity to fully consider their own needs and evaluate options. These traditional dynamics result in a status quo that does not shift to accommodate new programs or practices; instead, new programs and practices are changed to fit the system (Metz & Bartley, 2012). In order for policy to effectively enable practice in communities, it must be informed by practice. When policy-practice feedback loops are institutionalized within a system, they can promote systems change. Formal, transparent and ongoing bi-directional communication between rural communities and state and federal partners can help push the NRHA recommendations from paper to practice.
In addition to the creation of Practice-Policy Feedback Loops, funders and government agencies must invest in the development of general and innovation-specific capacity in rural communities. Successful implementation depends on capacity: the set of knowledge, skills and abilities required to deliver an intervention or program (Flaspohler, P. et al., 2008). Building and sustaining capacity is the foundation of implementation practice, because people, organizations and systems need to know how and be able to deliver an intervention in order for those in need to benefit from the intervention. Rural communities face challenges building and maintaining the capacity necessary to implement effectively. Limited capacity is one of the reasons that the vast majority of substance use treatment facilities and services are located in urban areas.
Building capacity is the first and foremost implementation need in rural America. Funders can support strengthening general administrative practices through funding overhead allocations and technical assistance, recognizing that fewer staff and lower capacity makes supporting new practices difficult for rural organizations. Similarly, funders can work with communities to create new approaches for building individuals’ capacity to deliver programs effectively. This may include funding streams for hiring or subsidizing new substance use professionals in rural communities through mechanisms such as the National Health Services Corps, or long term investment strategies for “growing” substance use professionals where they live – identifying community members who can become part of the workforce through training and coaching.
Effective Innovations
Few innovations – whether clinical practices, such as MAT, or public health practices, such as public awareness campaigns – are developed and tested in rural settings. There is frequently little information about which evidence-based or evidence-informed programs can achieve outcomes in the rural context. Rural communities therefore typically make choices to implement programs that are unknowns, or failing to find an evidence-based program that aligns with their need and context, create their own or borrow from other similar communities’ home-grown initiatives. (Smith, Adimu et al., 2016)
Funders, state agencies and researchers must collaborate with rural communities to co-create evidence-informed practices and models to address opioid use disorders that are usable and effective.
Selecting and translating appropriate innovations to be implemented in rural communities requires creativity and partnership. The NRHA recommendations include many options, some of which are well defined and others which are not yet so. For well-defined innovations with demonstrated effectiveness, such as MAT, funders must support translation and evaluation in rural communities. Rural communities must be supported to ‘think outside the box’ for how best to implement evidence-based strategies in their communities. The ‘hub and spoke’ model developed in rural areas should be expanded and evaluated, per the NRHA recommendations. Communities and state agencies can also think creatively about how to expand upon this model by using other effective rural service delivery models, such as the Mobile Medication Management model. When there are not well-defined existing models with demonstrated effectiveness in rural communities, such as the NRHA recommendation to develop community strategies to address the opioid epidemic, funders can identify programs developed by and in rural communities that are practice-based evidence, and seek to better understand the core components and outcomes of these interventions through research.
Enabling Implemetation
Fully implementing a well-defined evidence-based practice typically takes two to four years. (Metz, A., Naoom, S.F., Halle, T. & Bartley, L., 2015). Implementation takes time and proceeds through stages defined by best practices for the development and sustained use of Implementation Teams, infrastructure and data. Stage-based implementation is important regardless of context. Failure is likely when communities jump directly to implementing without taking adequate time to either explore need and assess fit and feasibility of a new program or build the necessary infrastructure required for implementation. Taking adequate time for implementation is particularly critical in rural communities where funds must be used as judiciously as possible to assure outcomes.
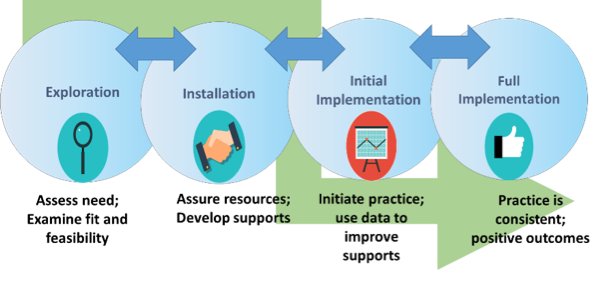
Our experience in rural communities indicates that implementation time lines must be extended. The necessity of building enabling context requires additional time. In particular, funders must support rural communities’ need for additional time and support for the early stages of implementation. Exploration of need, fit and feasibility must address aspects of proposed policies or practices that will require contextualization and translation for a rural community. Once a program or practice has been selected for implementation, funders can work with rural communities and training and technical assistance providers to explicitly identify and build infrastructure to fully install the new model in a community. Rural infrastructure needs are different than those found in urban communities. Taking the necessary time to proactively identify and build unique rural infrastructure needs, such as robust budgets for travel for both practitioners and MAT patients, will ensure implementation can be successful.
Taking time feels like a luxury when rural communities experience the opioid crisis viscerally every day. The ‘slow burn’ of intentional diagnostic and planning work can be frustrating in the face of great need and the sense of a ticking clock with time limited funds. Funders, policy makers and communities must acknowledge this tension and wrestle with the hard truth of implementation: without adequate time spent in exploration and installation, programs are unlikely to succeed. Our colleague in rural North Carolina referred to early implementation work as the challenge of “pay now or pay later – with interest.” We argue that rural communities cannot afford the interest rate associated with ineffective implementation of substance abuse services. Attention to implementation best practices can ensure communities can reap the benefits of research and policy that supports effective substance use prevention and treatment.
Resources
Return to Top | Download PDF Version | References