March, 2014
David Mee-Lee, M.D., Chief Editor, The ASAM Criteria
Senior Vice President, The Change Companies
A new edition of the Patient Placement Criteria for the Treatment of Substance-Related Disorders of the American Society of Addiction Medicine (ASAM) was unveiled October 24, 2013 in Arlington, Virginia. The new title is The ASAM Criteria – Treatment Criteria for Addictive, Substance-Related, and Co-Occurring Conditions. As the most comprehensive set of guidelines for assessment, service planning, placement, continued stay and transfer/discharge of individuals with addiction and co-occurring conditions, ASAM’s criteria are required in over 30 states and in Department of Defense addiction programs around the world. Many payers also manage care using the criteria that are the most intensively researched set of addiction placement criteria in the USA and Europe.
The other significant publication in behavioral health care published in May, 2013 was the new fifth edition of the Diagnostic and Statistical Manual of the American Psychiatric Association – DSM-5. Another significant publication just released in September, 2013 is the National Survey on Drug Use and Health (NSDUH) from SAMHSA, the Substance Abuse and Mental Health Services Administration. The results for 2012 reinforce what previous years’ data show – that millions of Americans needing addiction treatment are not identified; do not try to access services; and only about 10% actually get into specialty addiction services.
The new edition of The ASAM Criteria, DSM-5 and the NSDUH data are all significant given the current climate of healthcare reform. Consider the following data: The Affordable Care Act (ACA) is fully enacted in 2014, with potentially 30 million people now uninsured who could access health insurance. Not all will enroll and/or live in States that will not expand Medicaid to allow them to get health insurance. But there will still be millions more who have health insurance, even if it is just a fifth of those who eligible to be covered.
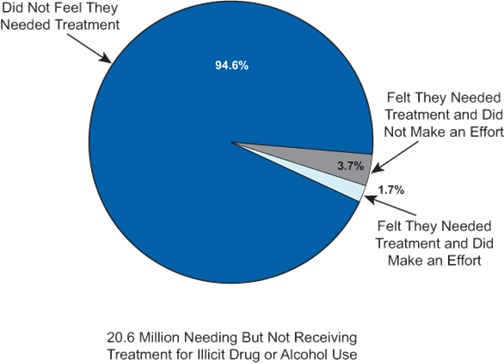
If there are millions more people who in 2014 can now be covered by health insurance with access to addiction treatment, how will addiction treatment agencies increase access to care when we already have waiting lists and can’t even meet treatment-on-demand now, for the 2.5 million people who did eventually receive specialty addiction treatment?
Perhaps you noticed that in this new third edition of ASAM’s criteria, the title is The ASAM Criteria – no “patient placement” in the title. That does not diminish the importance that the new edition still places on defining levels of care and admission criteria for placement in the broad continuum of care. But this edition ties in with ASAM’s definition of addiction that sees addiction as “a primary, chronic disease of brain reward, motivation, memory and related circuitry.” Thus the new edition is as much about guidelines for chronic disease management as it is placing people in programs.
In the context of healthcare reform and the data from the NSDUH and other such data, the new edition of The ASAM Criteria with related notes on DSM-5:
What’s New in DSM-5 and The New ASAM Criteria?
Implications in an Era of Healthcare Reform
While the specific admission criteria and levels of care have not essentially changed in The ASAM Criteria, there are some changes in how we designate the levels of care. Instead of Roman numerals for the levels, regular Arabic numerals are used. So what was once Level I or II services become Level 1 or 2 services and so on. DSM-5 also switched away from Roman numerals as in DSM-IV, in part so DSM could become a “living document” with changes and enhancements accessible through a subscription web-based version. Perhaps we will soon see version DSM-5.1 or DSM-5.2. The ASAM Criteria also has a web-enhanced subscription version for similar reasons.
Another significant change in terminology in The ASAM Criteria is to re-name “detoxification”. Since the liver detoxifies substances, but clinicians manage the withdrawal, the new edition changed to “withdrawal management” services instead of “detox” services. Often patients are placed in the most intensive and expensive level of withdrawal management, a hospital Level 4 service for three or four days to ensure they do not have withdrawal seizures. Then upon discharge or soon after, the person uses substances again and is confronted about using when they were already “detoxed.”
Actually the patient was treated just long enough to prevent seizures and then discharged, but his or her withdrawal was not managed and so they use again. The change to “withdrawal management” emphasizes the importance of using a continuum of withdrawal management services to support a person through both the physiological and psychological signs and symptoms of withdrawal. This may require a couple of weeks for some, not just a few days in hospital. Such withdrawal management can be done using the same or even less resources than are spent on a few days in Level 4 hospital which often has rates of up to a $1,000/day.
Here are a few more terminology changes in DSM-5 that clinicians will need to get used to:
No more multiaxial system (Axes I, II, III, IV and V) to document diagnoses, functioning and psychosocial factors – just list the diagnoses to reflect the whole person, not separating mental disorders from physical and general medical conditions.
No more "Substance Abuse and Dependence." Now use "Substance Use Disorder" with severities of mild, moderate, and severe.
No more “Not otherwise specified” (NOS) – now use “other specified disorder” to document the specific reason the client presentation does not quite fit a diagnostic category; or use “unspecified disorder” if the clinician chooses not to document the reason criteria for a disorder are not met.
Much time and resources are spent by clinicians and managed care organizations communicating back and forth in the treatment payment approval process. One of the goals of the new edition is to have The ASAM Criteria enhance assessment, placement and the care management processes for providers and payers. With an unsustainable trajectory of healthcare costs, we should all be managing care to use resources efficiently and increase access to care. When focused on assessing all six assessment dimensions of The ASAM Criteria and planning an individualized collaborative plan, clinicians are in fact managing care if the treatment level selected is the least intensive but safe level of care for the person.
This isn’t about placing a person in the least intensive level until they “fail” that level. This is about making sure we give people all the care they need, but not in a more intensive level than is clinically safe as that is wasteful of scarce resources. But also not to place them in a less intensive level of care that matches their severity and level of function. If they go to a less intensive level than is needed and end up getting worse that is not good for the patient and his or her family, but also not good for budgets as the person then ends up in emergency rooms or more acute care again.
The following decision flow outlines how to move from engagement of the client (“What do you want?”), to assessment of immediate and multidimensional needs; diagnosis then to service planning and level of care decision. The DSM diagnoses are necessary, but not sufficient to determine treatment needs and level of care. It is the multidimensional severity and function that is pivotal in placement criteria. This is the process in both care delivery and care management.

From Engagement,
Assessment,
Service Planning to
Level of Care
The ASAM Criteria Software, now in demonstration pilot testing phase, is slated to be released in the fall of 2014. The software will work hand in hand with the Criteria book to make the utilization review and care management process much more efficient for everyone involved – providers, payers and care managers.
So now you have a bird’s eye view of the new The ASAM Criteria and DSM-5. If you’d like to see more about The ASAM Criteria, visit www.ASAMcriteria.org for additional information on how to buy the criteria book; subscribe to a web-enhanced version, get Continuing Education credits in three eTraining modules; and download free articles on The ASAM Criteria. You can even download some PowerPoint slides on what’s new.
Orlando, Florida
April 10-13, 2014
David Mee-Lee, M.D. is a board-certified psychiatrist and is certified by the American Board of Addiction Medicine (ABAM). Based in Davis, California, he trains and consults nationally and internationally. Dr. Mee-Lee has led the development of the ASAM Criteria since the late 1980's. He co-authored the first and second editions and is Chief Editor of ASAM PPC-2R (2001) and the new edition of The ASAM Criteria (2013). He is also Senior Vice President of The Change Companies.