By Northwest Addiction Technology Transfer Center Network
SAMHSA’s Addiction Technology Transfer Center (ATTC) Network maintains a mission to accelerate the adoption and implementation of useful treatment and recovery practices by the addiction workforce. While that mission may be familiar to many at SAMHSA, there is continuing need to broaden awareness of the transformative potential of the work of the ATTCs among researchers, policymakers, workforce advocates, and the public at-large.
One means to broaden ATTC network familiarity among such audiences is through scientific publication, in which the rigor of conceptual ideas and methodological processes inherent in ATTC-sponsored projects is subject to stringent peer-review processes. A pair of recent scientific publications led by Bryan Hartzler, PhD—who serves as director of the Northwest ATTC, housed at the University of Washington’s Addictions, Drug & Alcohol Institute—are examples that may pique the interest of audiences less familiar with the ATTC network.
The first of these publications, freely available to the public as an open-access article through a Journal of Substance Use and Addiction Treatment special issue on Stimulants1 (https://www.jsatjournal.com/article/S2949-8759(22)00012-1/fulltext), describes a recent inter-agency partnership involving Oregon Health Authority, a statewide treatment agency, and the Northwest ATTC. This involved Dr. Hartzler providing implementation support to enable sustainable implementation of contingency management (CM) programming that demonstrated clinical effectiveness in increasing stimulant abstinence among clients of an opioid treatment program in Medford, OR. The other publication, a commentary in the prestigious American Psychological Association journal Clinical Psychology: Science and Practice2 (https://doi.org/10.1037/cps0000138), discusses dissemination considerations for cognitive-behavioral therapy as a frontline therapy for persons with substance use disorder.
A mutual focus of both articles is the transformative potential of technical assistance (TA), a term encompassing current ATTC network efforts. It includes universal TA where events like webinars promote workforce awareness of useful treatment and recovery practices, targeted TA with events like training workshops enabling individual workforce members to build knowledge and skill in a particular practice, and intensive TA in which systems-level changes are facilitated to enable organization-wide implementation of a particular practice. Through all such forms of TA, Dr. Hartzler suggests “the addiction workforce—ever diversifying in composition and the settings where they encounter clients with SUDs—stands to benefit from the broader dissemination of useful behavior therapies to assist clients in reducing substance-related harms”.2
What Does Intensive TA Look Like at the Northwest ATTC?
It is in the provision of intensive TA that the Northwest ATTC observes its most beneficial impacts on the addiction workforce. The noted articles each reference the pragmatic model that Northwest ATTC applies in providing intensive TA, which over the past five years has been collectively applied to support implementation of a dozen treatment and recovery practices in projects with community partners located in HHS Region 10 states of Alaska, Idaho, Oregon, and Washington.
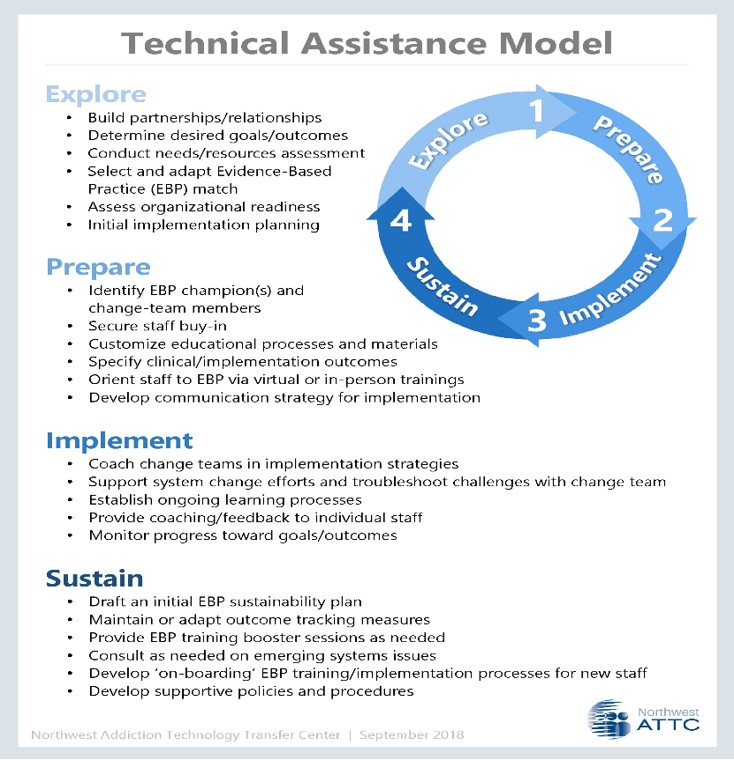
In providing intensive TA, the Northwest ATTC applies a phased Exploration-Preparation-Implementation-Sustainment (EPIS) framework3. Within this chronological framework, an initial exploration phase involves assessing the local needs and resources of the partnering organization, and adapting a focal treatment/recovery practice for customized use. The subsequent preparation phase involves preparing the organization’s systems and staff to implement the practice, oftentimes with staff exposed to online, in-person, or virtual
training. An implementation phase then provides additional, ongoing assistance—via organizational consultation, or individual coaching provided to clinical staff—as the practice is implemented on a provisional basis. The eventual sustainment phase often includes the provision of a project report, summarizing processes and outcomes, to aid a collaborative determination about whether and how the focal practice may be sustained in the future.
Publication as a Means of Sharing a Case Example
An additional benefit of scientific publication is the opportunity it presents to others to replicate successful work. As an example, the noted publication in the Journal of Substance Use and Addiction Treatment publication details the Northwest ATTC approach to intensive TA in a manner that invites other regional ATTCs, and more broadly any intermediary purveyor organization, to follow in supporting community-based CM implementation. This particular case example included SOR funding support from the Oregon Health Authority, and involved the Medford Treatment Center, a community-based opioid treatment program affiliated with Oregon Recovery and Treatment Centers, LLC.
A key component of the exploration phase in this project was a collaborative design process in which CM programming was customized to be both theoretically-sound and compatible with the local needs and resources of Medford Treatment Center. For any clinical practice like CM, achieving such compatibility in its initial design increases the likelihood of success in its initial implementation and sustainment over time.
A preparation phase next included Northwest ATTC guidance and resources, including:
A six-month implementation phase next occurred, with CM programming delivered with all stimulant-using clients, as stimulant abstinence had been chosen by leadership of Medford Treatment Center as the client behavior to be reinforced. During this period of active implementation, Northwest ATTC provided ongoing consultation and a digital resource library that Medford Treatment Center staff could freely access as needed.
The sustainment phase included examination of observed therapeutic impacts among CM-exposed clients in comparison to other Medford Treatment Center clientele not receiving CM. These impacts included significant effects, with CM-exposed clients showing: 1) an 11% higher rate of stimulant-free urine drug screens, and 2) a 14% higher rate of retention in services over the six-month period. On the basis of these findings as well as their anecdotal implementation experiences, Medford Treatment Center leadership chose to sustain this CM programming as part of its routine clinical services thereafter.
Growing a Forest, One Tree at a Time
Though the case example describes a single-site project, it may be useful to note here that this same intensive TA approach has since been applied with many other treatment settings seeking to institute CM and with similar success. Dr. Hartzler and colleagues state that they “hope this work serves as a helpful template…to design and sustainably implement CM programming that addresses individual treatment settings’ local needs and available resources”1.
Providing intensive TA in this manner is akin to the art of growing a forest, one tree at a time. As Dr. Hartzler notes, the ATTCs “as regionally based intermediary purveyor organizations linked in a national network, have a critical role to play given their shared mission to accelerate the adoption and implementation of useful treatment and recovery practices”2. By exposing new audiences through scientific publication to how those in the ATTC network are providing supportive and ultimately successful intensive TA, this forest has a chance for rapid growth.
References