April, National Minority Health Month, is being recognized this year with the theme “Accelerating Health Equity for the Nation.” Healthy People 2020 defines health equity as the “attainment of the highest level of health for all people.” To achieve this, it is essential to eliminate avoidable health inequities, systemic disparities in health care and in the major social determinants of health among social groups that have different levels of underlying social disadvantage.
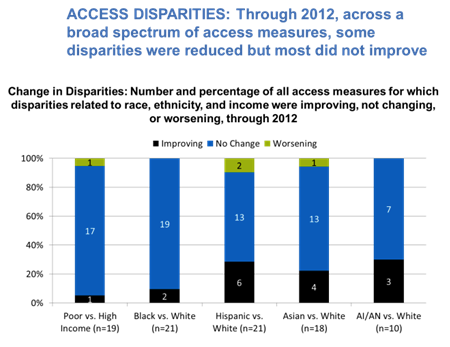
Health and behavioral health disparities are longstanding, challenging problems in the U.S. Each year, the HHS Agency for Healthcare Quality and Research issues the National Healthcare Disparities Report that provides a comprehensive overview of the quality of health care received by the general U.S. population and disparities in care experienced by different racial, ethnic, and socioeconomic groups. Progress in reducing disparities has moved at a snail’s pace: fluctuations from year to year may reflect such variable influences as health policy reform, an economic recession, shifts in population demographics or other non-health related events. But overall progress is unremarkable.
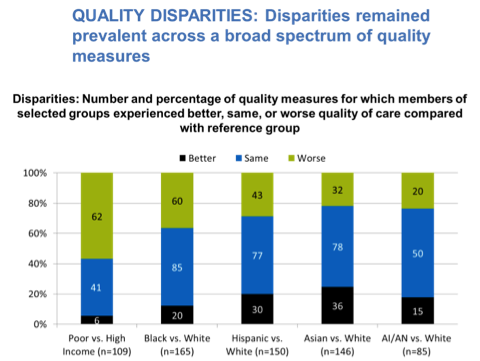
A typical comparison of health disparities among populations is reflected in the figure below with the current majority white group being the referent population.
Major policy reports, historical and current, have focused on heath and behavioral health disparities: the Heckler Report of 1965 documented severe disparities in the health of Black Americans; the 2001 Surgeon General’s Report on Mental Health: Culture, Race and Ethnicity identified gaps in prevent, treatment and research in mental health for diverse populations; the 2002 IOM Report on Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care underscored significant differences in access to care; the 2003 New Freedom Commission on Mental Health put forth recommendations for improving access, quality care and a workforce trained to work across cultures; the 2012 HHS Secretary’s Action Plan to Racial and Ethnic Disparities in Health Care called for disparity impact statements in the grant-making processes of the department; and HHS’s re-issuing of the enhanced National Standards for Culturally and Linguistically Appropriate Services In Health and Healthcare in 2013 re-focused attention on systemic, clinical and civil rights issues in equitable delivery of health care. Each report has been groundbreaking, elevating focus on disparities and highlighting various strategies to advance equity.
Building on each of these major policy reports, SAMHSA has taken a multi-pronged approach to advancing equity. SAMHSA’s earliest work focused on cultural competence and developing training and system change strategies to ensure that an organization’s policies, structure, practices and attitudes reflected attention and responsiveness to the cultures of the populations being served. More recently, SAMHSA’s Office of Behavioral Health Equity has implemented a data-driven, quality improvement approach to addressing disparities by requiring all grant programs to submit “disparity impact statements.” These statements must demonstrate how the grantee is improving access, service use and outcomes for targeted racial and ethnic populations in their grant catchment area. Achievement of the goals in the disparity impact statement is measured through required performance data and tied to the grantee’s funding. Through this approach, grantees are demonstrating more outreach and engagement strategies to reach underserved and historically excluded disparity vulnerable populations.
The Office of Behavioral Health Equity also uses a “network structure” to advance health equity. Launched in 2008, the National Network to Eliminate Disparities in Behavioral Health, the NNED (www.nned.net), was designed to harness the work of community-based organizations (CBOs) around the country serving diverse racial and ethnic communities. These CBOs are not grantees. Often, the impetus for the creation of the CBO was the lack of appropriate services for their communities, lack of engagement by mainstream behavioral health organizations, and an overarching social justice framework. These CBOs are community-driven, culturally focused, multi-service agencies, that have a primary focus on the provision of behavioral health services.
At the time of the NNED’s formation, network structures were being promoted as the answer to “wicked” policy problems. “Wicked problems” referred to problems that seem intractable, defy easy solutions, interact with other deep-seated social and economic conditions and often persist because the systems put in place to solve the problems actually hinder development of effective solutions. These problems present a special challenge to government as they cut across policy and service areas and resist “silo’ed” approaches.
The mission of the NNED is to “build, partner with, and sustain a national network of diverse racial, ethnic and cultural communities and organizations to promote policies, practices, standards and research to eliminate behavioral health disparities.” The premise underlying the NNED is that there are feasible, realistic strategies to reduce disparities. This knowledge and capacity lies within communities and the individuals that experience these inequities on a daily basis, and not solely in outside experts, researchers and policymakers. The knowledge, innovations and effective practices within these CBOs must be elevated and shared within and across communities and policymakers. It is through this collective approach that communities can advance a health equity agenda. The NNED also includes individual “affiliate” members that may be researchers, policymakers, behavioral health professionals, consumers and families and others with a vested interest in underserved communities. This diverse membership fosters new partnerships, e.g., among researchers and CBOs, or family associations and CBOs, county officials and CBOs, etc.
The functions of the NNED include:
A few examples of the work of the NNED are described below.
 NNEDLearn brings training in evidence-based practices, culturally adapted evidence-based practices and evidence-supported community-developed practices to NNED members. Offered annually over the past six years, NNEDLearn combines in-person training with virtual coaching. Teams from NNED organizations apply to participate in one of five training tracks that meet with the developer or master trainer for 2 ½ days, then meet virtually by teleconference over a five month period to get coaching on implementation of the practice, and maintain ongoing communication with the trainer and their training colleagues through a web-based discussion forum. Through this model, neaerly 700 staff in 150 organizations have been trained. This year, in March 2016, NNEDLearn offered training for 120 participants representing 25 CBOs in one of the following interventions:
NNEDLearn brings training in evidence-based practices, culturally adapted evidence-based practices and evidence-supported community-developed practices to NNED members. Offered annually over the past six years, NNEDLearn combines in-person training with virtual coaching. Teams from NNED organizations apply to participate in one of five training tracks that meet with the developer or master trainer for 2 ½ days, then meet virtually by teleconference over a five month period to get coaching on implementation of the practice, and maintain ongoing communication with the trainer and their training colleagues through a web-based discussion forum. Through this model, neaerly 700 staff in 150 organizations have been trained. This year, in March 2016, NNEDLearn offered training for 120 participants representing 25 CBOs in one of the following interventions:
(1) Motivational Interviewing;
(2) Project Venture: Prevention of Risky Behaviors for American Indian Youth;
(3) Familia Adelante: A Family Strengthening Intervention for Latino Families;
(4) Preventing Long-term Anger and Aggression in Boys and Young Men of Color; and
(5) Strengthening Intergenerational/Intercultural Ties In Immigrant Families, geared for Asian and Latino immigrant and refugee families. (For more information go to: http://www.nned.net/nnedlearn/)
 NNEDShare is a collaborative space on the NNED website to share resources and interventions to improve the delivery of behavioral health care in diverse populations, learn about resources and innovative community efforts across the country, and connect with peer organizations. NNEDShare includes innovative engagement and outreach efforts, public education campaigns, new or adapted practices, services, policies, organizational structures or business models. Some examples include: Depression Fotonovela: Development of a Depression Literacy Tool for Latinos with Limited English Proficiency; Café Hope Espresso Project: Job Training Program for Behavioral Health Clients; and
NNEDShare is a collaborative space on the NNED website to share resources and interventions to improve the delivery of behavioral health care in diverse populations, learn about resources and innovative community efforts across the country, and connect with peer organizations. NNEDShare includes innovative engagement and outreach efforts, public education campaigns, new or adapted practices, services, policies, organizational structures or business models. Some examples include: Depression Fotonovela: Development of a Depression Literacy Tool for Latinos with Limited English Proficiency; Café Hope Espresso Project: Job Training Program for Behavioral Health Clients; and
Shape Up! Barbers Building Better Brothers: A Sexual Health Intervention for Young Black Males in Philadelphia. For more information go to: http://share.nned.net/
The NNEDNote is a bi-monthly electronic newsletter that reports on upcoming federal and foundation funding opportunities, recent research studies, upcoming events, and related activities. If you are not already a NNED member, please consider joining the NNED. The NNED is also active in social media through Facebook, LinkedIn and Twitter.
While the month of April puts a focus on the health of minority populations, the work to end disparities and advance health equity is a year-round effort. No single effort, no short term effort will accomplish this goal. A promising approach is through a collective, comprehensive effort that focuses on both the service delivery system and the social determinants of community health.