 The ATTC Network is funded by SAMHSA and the author’s opinions do not necessarily represent the opinions of SAMHSA or the ATTC. We respectfully offer this article to encourage healthy discussion to advance our field.
The ATTC Network is funded by SAMHSA and the author’s opinions do not necessarily represent the opinions of SAMHSA or the ATTC. We respectfully offer this article to encourage healthy discussion to advance our field.
Sandeep Kapoor, MD, MS-HPPL
Assistant Vice President, Addiction Services
Northwell Health Emergency Medicine Services
Without mainstream advocacy, like we witness for heart disease, diabetes, and cancer, substance use disorders (SUD) have long been viewed as an “individual’s problem,” not as a healthcare issue deserving of championship. The alarming stigma that plagues the chronic medical condition of SUD has driven inaction in many healthcare arenas. The lack of investment, education, and humanistic individualized care has created industry-wide fractures in how we approach those with a SUD. The cries of our families and our communities fall on deaf ears — ears that are attuned to understand diseases of the heart, pancreas, and cells — though are unable to understand the science behind addiction. The lack of medical education fuels the lack of motivation to change, very quickly making SUD a problem for individuals, having to navigate on their own, without the support or empathy of others.
The journey we travel is populated by an inherent need for acknowledgement—that feeling of being heard, understood, respected, and valued. This simple human characteristic represents a commonality which should unite us, however, this trait equally and easily can create divides. Our ability to acknowledge, or discount, rests in the power of our words—utterances which, without delay, can create an environment unwelcoming to others. Though the positive value of words is readily appreciated when infused with affirmation, validation, and empathy, we tend to discount the power our words hold and underappreciate palpable effects of when our verbiage expresses judgement, shame, and disfavor.
The good news is that the healthcare industry is undergoing a long-necessitated swing, moving from directive care delivery to person-centric, holistic care. Over the years, we have seen a shift in recognizing the importance of understanding others. I believe this has been fueled by self-identification of our own individual needs—needs that we are now realizing we ourselves must fulfill in order to feel whole, to feel well, and to feel secure. Regardless of the progress made, which by all means should be applauded, there’s a long way to go on this journey. The thinking that someone is beneath us due to their struggles, are thoughts that have undoubtedly corrupted us, penetrating our language, and perpetuating the use of derogatory and stigmatizing expressions. George Orwell said, “If thought corrupts language, language can also corrupt thought.” Thoughts of superiority have distanced us from understanding the basic need we all have in common —the need for acknowledgement. These thoughts are fed by what we see and hear. The origins of these thoughts can be mapped to our socially primed stigmas, refined at our dinner tables and reinforced within our workplaces, informed by years of misinformation, permitting the continued devaluation of others, including individuals struggling with a SUD.
The cyclical nature of this detrimental equation is one that needs focus, discovery, and resolve. As healthcare professionals, sworn to provide unbiased, non-discriminatory, high quality care, we all have power in this equation. We should not ignore the past and current states of disparate and discriminatory practices, but better yet, we should memorialize them, and use them as a source of communal motivation to act, to innovate, and to correct our wrongs of the past. We should openly and jointly take accountability and make this “our problem.” We need to leave underwhelming ways in the rearview mirror and evolve to raise health for all. Regardless of the paralyzing nature of this complicated equation, there are starting points each one of us can incorporate into our approach. The benefit of this being a multifactorial calculation is that there is no shortage of opportunities to start making a difference, at a personal-, departmental-, organizational-, industry-, and community-level.
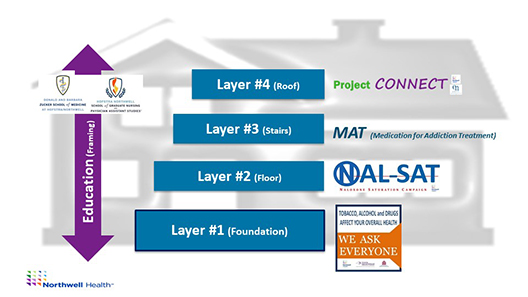
Action is possible. My team and I have the privilege of working to motivate the largest healthcare organization in New York State to humanize and address substance use as part of usual care. The team-based, interprofessional, multidisciplinary collaborative efforts have propelled our organizational mission to normalize and accept substance use as a healthcare issue. At Northwell Health, we have implemented a layered approach to humanizing and addressing substance use as part of usual care. Our “Pathways to Recovery” programming is constructed using a house of strategies with layers of sustained processes and protocols that have been embedded into workflows in order to acknowledge those struggling with substance use. We are now, systematically, offering opportunities for others to be heard, valued, and to be treated with respect:
Layer 1: Our Screening, Brief Intervention, and Referral to Treatment (SBIRT) program is Northwell’s foundational strategy for addressing substance use in all clinical arenas, including 18 emergency departments, 14 inpatient hospitals, and a robust ambulatory network. By providing opportunities, universally to all, patients are encouraged to discuss with their trusted clinical teams how the use of alcohol, drugs, and/or tobacco are impacting them. Similar to checking a patient’s blood pressure at every touchpoint to understand risk of heart disease, we view SBIRT as an opportunity to measure a “vital sign” for SUD, facilitating a better understanding of self-identified consequences of one’s substance use, motivations to make changes, and willingness to partner in seeking reduction of use, well-being, and/or recovery.
Framing: Education is the framework for the house of strategies. Educating our current and future interprofessional clinical team members on how to humanize the topic of substance use and empowering them with the tools to address and treat this disease process is critical to motivating a shift in organizational and industry-wide culture.
Layer 2: Our Naloxone Saturation Campaign (NAL-SAT) allows clinical and non-clinical team members to provide patients, their families and friends, staff, students, and community members, education on opioid overdose prevention, recognition, response, and rescue. The unrelenting increases in opioid overdoses year after year fuels our motivation to dispense naloxone rescue kits at point of care, and at no-cost thanks to a partnership with the New York State Department of Health.
Layer 3: Medications for Addiction Treatment (MAT) are available, as are medications for other chronic medical conditions. Addiction treatment need not be delayed, so we have created protocols to initiate MAT in our emergency departments, supported by a next-day follow-up at one of our Northwell Addiction Treatment facilities.
Layer 4: Project Connect, a collaborative endeavor representing a programmatic marriage between Northwell Health and a community-based organization (Central Nassau Guidance and Counseling), provides 120 days of external care navigation and support for patients dealing with SUD. With the understanding that it is difficult navigating the landscape of addiction care, the ebbs and flows of personal motivations, and the well-defined barriers to care such as access, transportation, and finances, we are creating avenues for continuity of care so that individuals aren’t left to fend for themselves once they leave the four walls of our clinical settings. Modeled after care navigation protocols for cancer care and joint surgeries, we are demonstrating that individuals with the chronic condition of SUD will benefit from chronic care navigation.
WE ARE NOT ALONE! — That is very freeing to shout and share! There are countless colleagues and health organizations that are far ahead of us, and many that are just starting. We need to coalesce and share our journeys to illustrate that action, advocacy, and change is possible. Recently, I had the honor to share my journey with school-based health professionals on identifying the value of SBIRT, and we explored how value can be measured even in the absence of reimbursement. The conversation served to be validating, as for almost eight years, my team and I have been on a journey to destigmatize, to normalize, and to humanize substance use utilizing SBIRT as a primary driver. It was a moving dialogue that facilitated my reinvestment in the thinking that individually, we all have the power to serve as ‘Conduits of HOPE’ for a disease process that still remains hopeless for far too many. Hope can be delivered, and as we strive to reframe and harmonize thinking and language revolving around SUD, we must accept the role acknowledgement plays in caring for others. Are you ready? Let’s partner to motivate our industry at-large to manifest consistent messaging and protocols affirming “YOU ARE NOT ALONE” to those dealing with substance use disorders. #InThisTogether
--------------------------
Sandeep Kapoor, MD, MS-HPPL is Assistant Vice President, Addiction Services for Northwell Health Emergency Medicine Services; Director, Screening, Brief Intervention and Referral to Treatment (SBIRT) at Northwell Health; and Assistant Professor of Medicine, Emergency Medicine, and Science Education at Zucker School of Medicine at Hofstra/Northwell.
[email protected] | Twitter: @KapoorMedEd
--------------------------
Additional reading resources: