"Without inspiration the best powers of the mind remain dormant. There is a fuel in us which needs to be ignited with sparks."
~ Johann Gottfried Von Herder (1744 –1803)
Patients in treatment are often intimately familiar with pain and punishment. This is one reason motivational incentives – positive reinforcements provided for taking incremental steps on a long, often arduous path of recovery – can be a powerful approach.
Additionally, the clinical use of motivational incentives (also called contingency management) has been honed through decades of research, resulting in a powerful intervention shown to improve patient retention and engagement, increase abstinence, and enhance overall recovery experiences in substance abuse treatment. It can also transform treatment environments. Since implementing motivational incentives, says Martin Gaffney, Director of Elmhurst Hospital Center in New York, "the whole environment, the whole ambience of the clinic has essentially changed in the last five years." (Motivational Incentives Suite , NIDA/SAMHSA-ATTC, 2011).
Although the use of motivational incentives has a long and consistent track record of effectiveness, implementation has not been as widespread as expected. In part this is due to resistance, which often shifts with increased understanding of the theory and principles supporting clinical application of motivational incentives, and through direct experience with its power to initiate change. In fact, armed with new knowledge, practitioners can often immediately begin improving and augmenting the ways in which they use incentives.
This three-part series will provide an introduction to motivational incentives (hereafter called M-Inc), including a discussion of benefits and challenges, supporting research, core concepts and principles that govern clinical use, and stories from an ongoing national campaign to help providers consider and implement M-Inc.
M-Inc is one of several evidence-based interventions the Addiction Technology Transfer Network features in training and technical assistance. In 2007, however, the Network increased its focus on M-Inc by joining the National Institute of Drug Abuse in launching a national campaign to raise awareness, knowledge, and interest in using incentives as an adjunct therapy to treat substance abuse disorders. The campaign featured a new toolkit of resources: Promoting Awareness of Motivational Incentives (PAMI).
Following a groundswell of interest from the field, and rich feedback and lessons learned, the PAMI toolkit was re-designed and updated, and two companion products added, to create a more advanced suite available at no charge to the field. The suite is the most recent offering from the National Institute of Drug Abuse (NIDA) "Blending Initiative", which partners Addiction Technology Transfer Center experts and NIDA researchers to develop and disseminate evidence-based tools for the field. The Motivational Incentives Suite includes three core parts: 1) the PAMI toolkit (2nd edition, 2011); 2) MI: PRESTO a self-paced, interactive on-line course designed to help providers implement and customize M-Inc; and, 3) MIIS (Motivational Incentives Implementation Software). For more details, and internet links, see "Resources" below.
This series will draw from the new Motivational Incentives Suite, which features a low-cost approach to using incentives shown to be effective through the most widespread research project on M-Inc conducted to date (discussed at the end of this article).
Recovery is a long, often difficult journey and the M-Inc program helps tip the balance (decision scale) by providing positive reasons to make next steps a little bit easier. A M-Inc program is used as a supplement to other therapeutic clinical methods. It restructures the motivational environment by providing immediate positive reinforcement (e.g., vouchers, goods, or privileges) to patients for reaching concrete targeted behaviors. Research has shown that this helps ambivalent patients move toward the changes treatment requires.
Motivational Incentives and Contingency Management. Contingency management (CM) approaches were first used in the 1960s, based on B. F. Skinner's work (1953, 1983). Skinner, who coined the term operant conditioning, proposed that reinforced behaviors are more likely to re-occur. His idea was that behavior can be learned and changed through the use of reinforcement or punishment (i.e., a stimulus-response pattern is reinforced and the individual is conditioned to continue to do the reinforced behavior, or if punished lessen punished behavior). The strategic nature of operant conditioning is highlighted in a comparison to classical conditioning, which refers to an involuntary or automatic response (behavior) to a stimulus. For example, patients with substance use disorders are often automatically triggered to crave alcohol or drugs by stimuli in their environment.
Maxine Stitzer, a pioneer in the application of behavioral analysis and behavioral therapy principles to drug abuse, offers a clear description of operant conditioning in the new video included in the Motivational Incentives Suite (NIDA/SAMHSA-ATTC, 2011): "(In) the very, very basic operant conditioning model you have a target behavior; you have a reinforcer; you link them together through a contingency; and, as B.F. Skinner had shown, you can increase the frequency of that behavior you're reinforcing." This is the basis of Contingency Management.
More recently the term motivational incentives is being used to emphasize that incentives are used to promote desirable or positive behaviors and to address client ambivalence. While the terms CM and M-Inc are often used interchangeably, they differ in that a CM program may include different types of contingent responses to target behaviors (including punishment and negative reinforcement), whereas M-Inc refers to a model that uses positive reinforcement, as defined below.
According to Scott Kellog, et al (2007) "While all kinds of models have been tried in addiction treatment settings, positive reinforcement schedules are increasingly the norm. In large part, this is the case because they are therapeutic and enjoyable for both patients and staff. Negative reinforcements and punishments, while effective at times, are unpleasant to use and may result in patient dropout (Stitzer et al, 1984) and other forms of resistance (Kazdin, 1994). Punishment, in general, has not been a very effective method in substance abuse treatment (McLellan, 2001)." Therefore, to understand M-Inc, it is important to understand what is meant by positive reinforcement, and how it compares to other types of behavior modification tools.
Reinforcement versus Punishment. The core difference between reinforcement and punishment is not so much whether it is pleasant or unpleasant, but whether the goal is to increase or to decrease the likelihood of a behavior. The goal of reinforcement is to increase the occurrence of a behavior, while the goal of punishment is usually to decrease the occurrence of a behavior. Also, punishment frequently involves the presentation of some kind of aversive stimuli when the undesired behavior occurs (e.g., getting a speeding ticket or a drug court sanction).
Positive versus Negative Reinforcement. Positive reinforcement involves the presentation of a stimuli (such as a voucher, tangible desired object, or clinic privilege) after a behavior occurs. Negative reinforcement involves the removal of a stimuli after a behavior occurs, usually associated with loss or pain (e.g., verbal reprimands being stopped after an adolescent cleans his room, or the repetitive "ding ding" sound a car makes until a seat belt is fastened, or the frequency of submitting urine samples is decreased after a period of submitting all negative samples).
In summary, positive reinforcement strategies are designed to increase the occurrence of a specific, desired behavior by breaking a larger goal down into smaller steps and reinforcing each of the steps. Furthermore, reinforcers are often given at a high rate of frequency for small, manageable instances of behavior change, and as close in time to the occurrence of a target behavior as possible, with the intent to make the behaviors easier to learn. For example, in a treatment setting, a patient might receive an incentive for attending each group session rather than needing to attend all group sessions before reinforcement is provided.
Motivational Incentives versus Motivational Interviewing. M-Inc is often confused with Motivational Interviewing (MI), another evidence-based practice. A commonality they share is that both aim to address a patient's ambivalence about extinguishing or reducing alcohol and other drug use – e.g., on the one hand patients may be experiencing some of the negative consequences of using (such as legal difficulties, family stress, and health problems), while on the other hand they still feel the lure of the excitement, pleasure, and reduction of psychic pain associated with drug use. While both M-Inc and MI work on this ambiguity, their methods and goals differ.
With motivational interviewing – a set of therapeutic skills that needs to be developed and practiced by a clinician over time and under clinical supervision – a therapist aims to work with a patient's ambivalence to create inner conflict (dissonance) in order to help him or her make a decision to pursue a path toward recovery.
M-Inc, which generally requires less training and practice, is used adjunctively with the therapeutic relationship and other treatment interventions. It uses positive incentives aimed at modifying a specific behavior; offering an immediate and tangible reward for engaging in health-promoting behavior helps a patient resolve his or her ambivalence about continued use. According to Kellog et al (2007): "Contingency management treatments ... seek to reach this end by reducing the relative value of the contingencies that support drug use through increasing the incentives that support abstinence. As abstinence grows in attractiveness, drug-using behavior should diminish in desirability."
More specifically, M-Inc not only focuses on resolving ambivalence, but during a crucial time in recovery where other forms of positive reinforcement may be sorely lacking.
Scott Kellog and his colleagues (2007) state: "A number of writers have emphasized the importance of making treatment attractive and reinforcing (Bickel et al., 1998; Marlatt & Kilmer, 1998). This may be particularly important if, as Greaves (1974) has argued, addictive people frequently have disturbances in their ability to feel and experience pleasure. For many, it may be a deficit in pleasure... which is the force that drives addictive behavior. Certainly patients seem to respond when a general culture of affirmation and support is integrated into a program that uses incentives. One of the reasons why this is important is because the recovering person may, in fact, be in a state of deprivation. That is, many of the benefits of recovery do not immediately come to those who have stopped using. In fact, they may have given up what they perceived as the benefits of using, only to find that are now faced with a whole new array of difficulties. Ultimately, the goal is for patients to find naturally-occurring reinforcers."
"While aversive or punitive methods have been used to reach goals, the systematic use of positive reinforcements, or pleasurable consequences, has been associated with humanistic efforts to improve problematic individual or social conditions." (Kellog et al, 2007)
An early example of incentives used in a humanizing effort can be found in mid-19th century Australia, where a reformer named Alexander Maconochie used a system of positive reinforcements and points to transform part of a prison complex, at a time Australian jails were known for brutality (Kazdin, 1978; ElectricScotland, 2005). Despite favorable results, and praise by some for his benevolence and humanity, Maconochie faced constant resistance and was eventually transferred to another prison, where he was criticized for his methods and unjustly dismissed. Maconochie's methods went on to have an immense impact on Western penology; and although he came to be known as the "Father of Parole", he died in ill health still campaigning against resistance for reform.
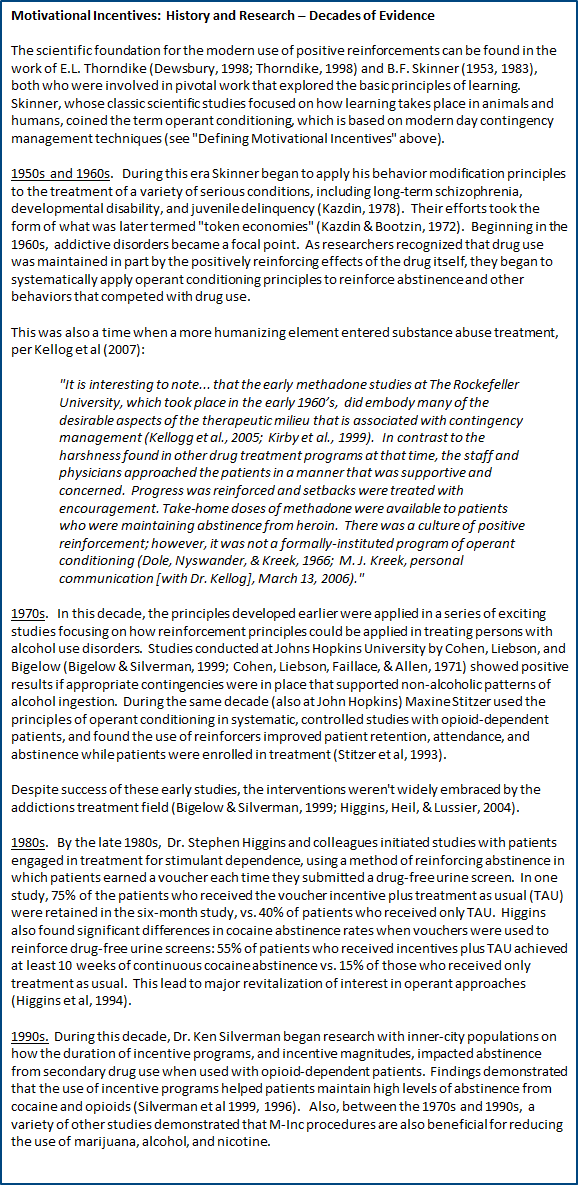
For more about the history of M-Inc, and the decades of research that support its effectiveness, please see the text box "Motivational Incentives: History and Research – Decades of Evidence" at the end of this article.
Following many decades of research, present day studies continue to find positive results through the use of M-Inc. Most recently, the NIDA Clinical Trials Network (CTN), a nationwide collaboration between addiction researchers and community-based treatment programs (CTPs), completed a study entitled Motivational Incentives to Enhance Drug Abuse Recovery. MIEDAR was based on Nancy Petry's work (Petry, 2000; Petry & Martin, 2002), which explored methods of delivering incentives that would reduce costs without sacrificing demonstrated effectiveness. In older voucher-based incentive delivery systems, for example, patients always received a tangible reinforcement immediately following a target behavior. Petry altered this methodology with her "Fishbowl" technique, which provides intermittent reinforcement, an approach that is both cost effective and improves outcomes (Petry, 2000; Petry et al, 2000).
The primary aim of MIEDAR was to study the use of lower-cost M-Inc for reducing stimulant use among patients receiving treatment at either methadone clinics (one arm of the study) or medication-free outpatient settings (the second arm). In all, about 800 patients were enrolled in both arms of the study, making MIEDAR the largest, multi-site trial of M-Inc conducted to date. The study yielded several positive findings, with the main outcomes generalized, as follows (PAMI 2nd Edition, 2011 [Trainer Guide]):
An area where more research is needed is the duration of time incentives need to be used to ensure positive impacts achieved are maintained once incentives are stopped. According to Donald Calsyn, a Professor of Psychiatry and Behavioral Sciences at the University of Washington, and a researcher for the Pacific Northwest Node of the NIDA Clinical Trials Network: "In many CM studies, but not all, the positive effects from CM disappear when the incentives go away. It is not clear if one needs to plan on providing incentives indefinitely, or if the length of the CM intervention in most studies was inadequate to get long term effects with incentives removed.... This does argue for selecting target behaviors that affect more short term goals such as incentivizing attending orientation sessions or IOP sessions, since these are time limited goals that have structured end dates after which incentives would no longer be provided."
M-Inc, with deep historical roots in behavior analysis and operant conditioning, are part of the advancements in evidence-based treatment for substance abuse and mental health disorders. The use of incentives, when implemented correctly, is supported by decades of effectiveness research. The large-scale NIDA CTN MIEDAR study was pivotal in demonstrating that M-Inc could be delivered at a significant reduction in cost without a corresponding loss in effectiveness. This has resulted in M-Inc being more accessible – and acceptable – to treatment programs.
The successful outcomes of the MIEDAR Study led to the creation of the original PAMI toolkit, followed by the updated Motivational Incentives Suite (NIDA-SAMHSA-ATTC, 2011) featured in an ongoing NIDA/ATTC national awareness campaign to help practitioners understand and consider adopting evidence-based M-Inc interventions.
Per Kellog et al (2007): In what may be seen as an example of principle-based dissemination, one of the central goals of the NIDA/ATTC awareness project is to familiarize clinicians and administrators with the core principles involved in designing and implementing a motivational incentives program. The concept is that if treatment centers are willing to design interventions that incorporate the seven principles... then they are on a path toward creating an effective program."
Part 2 of this series will review the seven core principles of M-Inc, including how they play out in different types of M-Inc programs, and considerations for implementation.
Series Author: Lynn McIntosh, BA
Series Editor: Traci Rieckmann, PhD, NFATTC Principal Investigator, is editing this series.
The Addiction Messenger's monthly article is a publication from Northwest Frontier ATTC that communicates tips and information on best practices in a brief format.
Northwest Frontier Addiction Technology Transfer Center
3181 Sam Jackson Park Rd. CB669
Portland, OR 97239
Phone: (503) 494-9611
FAX: (503) 494-0183
A project of OHSU Department of Public Health & Preventive Medicine.
Additional Information: