This was a two-day event consisting of an SBIRT Scale-Up policy meeting and intensive training workshop. The policy meeting was requested by the National Department of Health and was hosted by the South Africa HIV ATTC in the city Cape Town. The South Africa HIV ATTC’s collaboration with multiple agencies in SBIRT framework development this month has led to excitement from national stakeholders to observe and disseminate the training. The initial framework design was a collaborative creation aimed at the integration and scale-up of evidence-based SBIRT in mental health and HIV health programming. The intention of this meeting was to use scientific research to support the ongoing review of policy and implementation of SBIRT in South Africa.
Day 1 was a meeting with national stakeholders to discuss policy level possibilities related to SBIRT and how it impacts adherence support, retention, and viral suppression in people living with HIV.
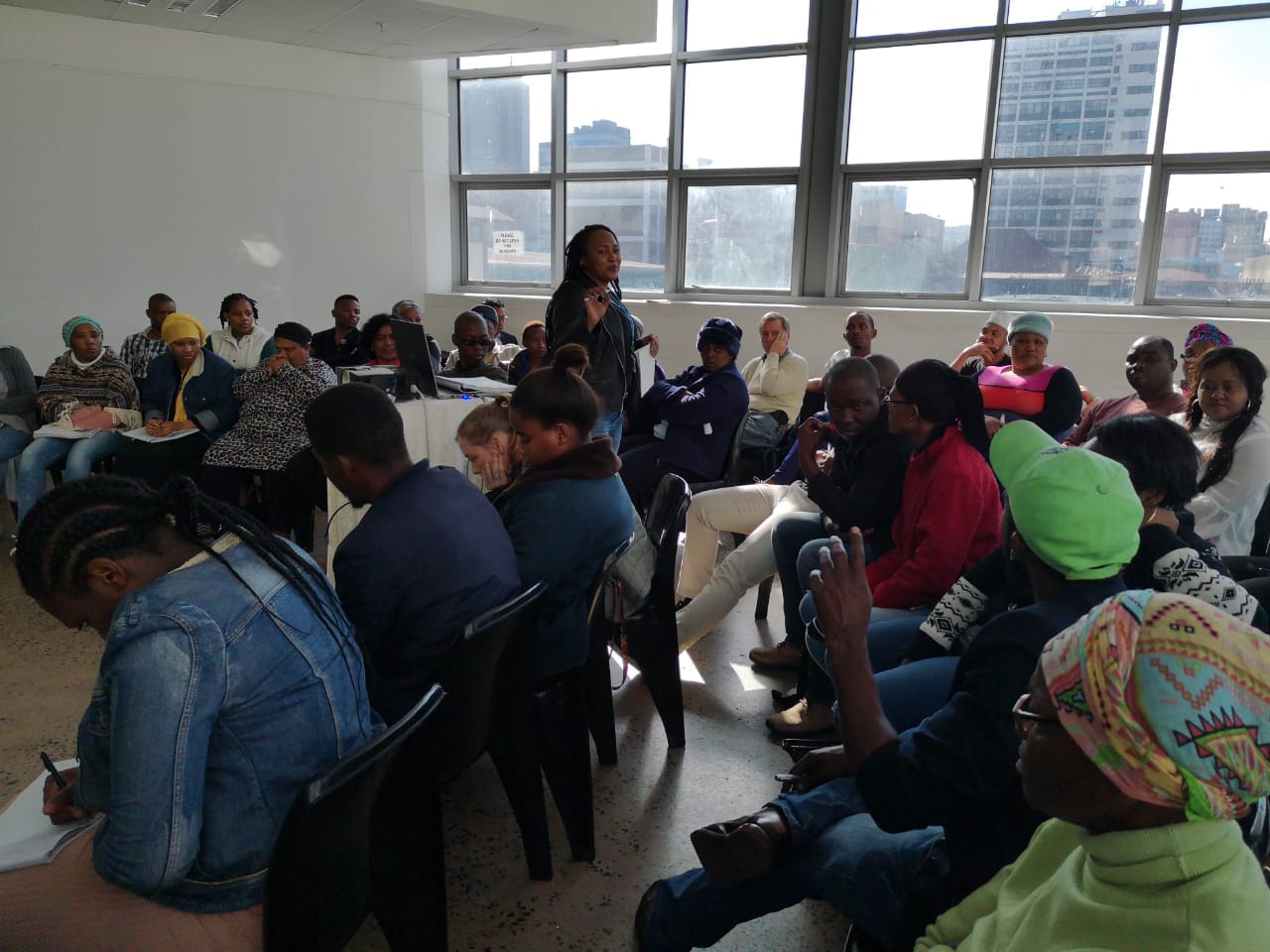
Day 2 was an intensive SBIRT training course stimulated by an initial request for such a training by MSF, which was attended by health professionals from multiple organisations across South Africa. There was an overview of screening tools and Motivational Interviewing followed by breakaway sessions showing where SBIRT can be applied to realistic scenarios. Attendees of the Day 1 meeting were invited to attend Day 2 activities to observe how the South Africa HIV ATTC administers SBIRT training.

This in-depth mental health training is a six-part series for health professionals and lay workers at the Denis Hurley Centre. The Denis Hurley Centre serves thousands of homeless, refugees, and people living with HIV and TB.
Attendees of this training gained knowledge around cultural competencies to better conceptualise the circumstances and care of their patients in order to improve HIV treatment outcomes through strategies such as increased detection and intervention of HIV and co-occurring mental, alcohol and other drug use disorders.
Attendees of this training gained knowledge about common mental and behavioural disorders, particularly mood and anxiety disorders. After this training, providers could better conceptualise the circumstances and care of their patients in order to improve HIV treatment outcomes through strategies such as increased detection and intervention of HIV and co-occurring mental and behavioural disorders.
Attendees of this training will gain knowledge about common psychotic disorders, intellectual disabilities, as well as suicide and aggression. The training particularly focuses on how these many different disorders can compound with HIV. After this training, attendees will better conceptualise the circumstances and care of their patients in order to improve HIV treatment outcomes through strategies such as increased detection and intervention of HIV and co-occurring mental and behavioural disorders.
Attendees of this training will gain knowledge about treatment and management of substance use disorders and mental illnesses. Those who attend this training will learn how to screen for mental health and substance use disorders and interpret the results of screening tools in order to improve HIV treatment outcomes through detection and intervention of co-occurring alcohol and other drug use among people living with HIV.
Attendees of this training will gain knowledge about treatment and management of common illnesses and issues associated with HIV/AIDS. Those who attend this training will learn how to interpret the results of screening tools in order to improve HIV treatment outcomes through detection and intervention of HIV and other co-occurring illnesses.
Attendees of this training will gain knowledge about treatment and management of common mental health illnesses and associated healthcare pathways related to those illnesses. Those who attend this training will learn about the Mental Health Care Act, hospital admissions and role players, the admission pathway and process, and non-specialist worker experiences.

TB HIV Care is an organisation that addresses the prevention, identification and treatment of HIV and TB in the general population as well as in key populations such as sex workers and people who inject drugs. This four-day training was particularly for TB HIV Care Trainers, who will cascade the training to lay workers, social workers, nursing staff, auxiliary social workers, and admin staff, with the ongoing supervision of the South Africa HIV ATTC. Additionally, this training was to help TB HIV care make their continuum of care more mental health responsive. Topics focused on psychotic, substance use, and mental disorders as well as psychosocial issues affecting vulnerable individuals. Attendees gained knowledge around cultural competencies to better conceptualise the circumstances and care of their patients in order to improve TB and HIV treatment outcomes. Strategies discussed in training included increased detection and intervention of co-occurring mental, alcohol and other drug use disorders. The MHPSS professionals that attended this training learned how to identify mental health and substance use disorders in order to improve HIV treatment outcomes through detection and intervention of co-occurring alcohol and other drug use among children and youth.
This four-day training was for Community Media Trust (CMT) and Aids Foundation South Africa (AFSA) professionals and Maternal Adolescent and Child Health (MatCH) subgrantees working with child orphans and vulnerable children. Attendees gained knowledge around cultural competencies to better conceptualise the circumstances and care of their patients in order to improve HIV treatment outcomes through strategies such as increased detection and intervention of co-occurring mental illness, alcohol and other drug use disorders. The training also focused on identifying other mental disorders and infectious diseases that frequently occur alongside substance use disorders. Providers that attended this training learned how to screen for mental health and substance use disorders and interpret the results of screening tools in order to improve HIV treatment outcomes through detection and intervention of co-occurring alcohol and drug use among adolescents at risk.

This training was for the KwaZulu-Natal Department of Health, Directorate for Mental Health and Substance Abuse. District surgeons, heads of department, and medical practitioners in attendance gained knowledge and skills in assessing and screening for mental health substance use disorders, brief interventions, as well as problem solving techniques. Attendees learned strategies to improve HIV treatment outcomes through detection, brief interventions and referral to treatment for alcohol and drugs. This training is very important as it kick starts an exciting new collaboration plan between the South Africa HIV ATTC and KZN Health.
Regional Psychosocial Support Initiative (REPSSI) is a non-profit organisation working to lessen the social and psychosocial (emotional) impact of poverty, conflict, HIV and AIDS among children and youth in South Africa. The purpose of this training was to help REPSSI design their HIV and Adolescent Psychosocial Support Programmes to be more mental health responsive. Topics focused on psychotic, substance use, and mental disorders as well as psychosocial issues affecting vulnerable individuals. Attendees of these two sessions gained knowledge around cultural competencies to better conceptualise the circumstances and care of their patients in order to improve HIV treatment outcomes through strategies such as increased detection and intervention of co-occurring mental, alcohol and other drug use disorders. Additionally, attendees learned how to identify mental health and substance use disorders in order to improve HIV treatment outcomes through detection and intervention of co-occurring alcohol and other drug use among children and youth.

This training was for TB HIV Care, Health Systems Trust (HST), and Maternal Adolescent and Child Health (MatCH); organisations that are District Support Partners for PEPFAR. This training was attended by mental health lay workers who work in HIV and TB settings. The first part of training was an introductory mental health training to introduce contextual competencies related to the treatment of mental and substance use disorders and to introduce basic symptoms of mental disorders. Providers that attended this training learned cultural competencies to contextualise the circumstances and care of their patients in order to improve HIV treatment outcomes through strategies such as increased detection and intervention of co-occurring mental, alcohol and other drug use disorders. The second part of training was a moderate-level mental health and substance use disorders training to identify other mental disorders and infectious diseases that frequently occur alongside substance use disorders. Providers that attended this training learned how to screen for mental health and substance use disorders and interpret the results of screening tools in order to improve HIV treatment outcomes through increased detection and intervention of co-occurring alcohol and other drug use.
This training was for Lifeline Durban, an organisation that conducts HIV testing, assessment, and counselling, in order to improve provider skills in motivational interviewing. This training targeted HIV non-specialists, including social workers, social auxiliary workers, and lay counsellors and served as a pilot for a national roll-out of our task-shifting training strategy. Providers that attend this training learned how to promote behaviour change in PEPFAR priority populations in order to improve HIV treatment outcomes through strategies such as increased HIV adherence, reduced alcohol use, and reduced drug use.