June, 2013
By Doug Dormer
The business of addiction and mental health treatment is under immense pressure. Demand continues to exceed capacity while funding from all sources is being reduced. People with mental health and addiction disorders have higher rates of comorbidities including diabetes, COPD, hypertension and cancer, not to mention HIV/AIDS and hepatitis C. The direct and indirect cost to society and to the healthcare system is extraordinary.
Yet addiction and mental health treatment works. Treatment of bipolar disorder, major depression, panic disorder, OCD and schizophrenia has been shown to improve health at rates that compare 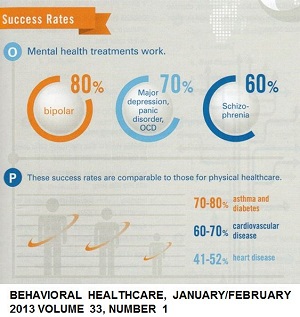 favorably to treatment of asthma & diabetes, cardiovascular disease and heart disease. Advances in neuroscience have increased our understanding of addiction as a brain disease; new treatments are emerging to treat it more effectively. Still, in some states, it is estimated that as few as 10 percent of the people who could benefit from addiction treatment actually receive it.
favorably to treatment of asthma & diabetes, cardiovascular disease and heart disease. Advances in neuroscience have increased our understanding of addiction as a brain disease; new treatments are emerging to treat it more effectively. Still, in some states, it is estimated that as few as 10 percent of the people who could benefit from addiction treatment actually receive it.
At the same time, new responsibilities, such as the Medicaid Health Home and SBIRT (Screening, Brief Intervention and Referral to Treatment) impose both opportunities and obligations that only these organizations can address.
Which is why it is amazing that for so many organizations, the elephant in the room is survival itself. In these times of both peril and opportunity, can we find a model for sustainability that will allow us not just to survive but also to thrive? The answer is yes, we can find models for sustainability, models where the question of operational efficiency
in service delivery becomes critically important. Health Information Technology (HIT) offers many tools that can contribute to your organization’s long term success and sustainability.
What is health information technology?
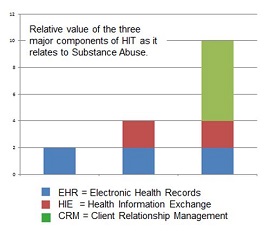
Health Information Technology actually consists of three different kinds of technology:
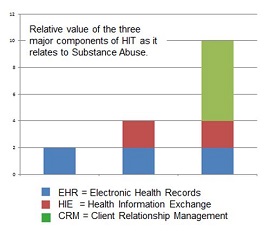
- Electronic Medical Records (EMR), clinical and practice management software that essentially move traditional paper-based practices to electronic ones.
- Health Information Exchanges (HIE), which allow behavioral and physical health providers to exchange personal health information with each other more efficiently.
- Patient Engagement Systems, including patient portals, personal health records and emerging mobile applications, which use technology to directly influence the way clinicians deliver service.
Most organizations find that adopting electronic medical records is of limited value. In fact, some providers find that EMR systems alone can hinder their operational efficiency, taking the focus off the patient and adding time-consuming steps to each patient encounter. Adding an HIE component can reduce the time and resources needed to share information among providers, but with only a modest impact on operational efficiency and sustainability. The real value comes from adding the patient engagement component that allows providers to communicate with patients in a new way. Patient engagement systems also bring added value to patients and their families.
Perceived barriers to HIT
- “It’s an all or nothing deal.” You have to have an EMR system in order to participate in an HIE or offer a patient engagement system. While eventually organizations will need all three components, each can be delivered independently, depending on the ability of the parties.
- “Security and privacy risks, particularly 42 CFR Part 2, are just too daunting.” That’s just plain wrong. While security and privacy are paramount, both the ONC and SAMHSA support carefully designed solutions that address the risks.
- “We just don’t have the IT staff to support this.” A valid argument, but there are ways around it. With the increase in hosted solutions, the burden on the organization can be quite manageable. Also, we’re seeing a number of regional coalitions and state associations acquire and manage technology on behalf of members. One way or another, staffing should not be a barrier.
- “My participants just aren’t up to this kind of technology.” They don’t have access to computers, their reading level is too low, and they don’t have the attention capacity to accomplish these tasks consistently. For example, it is one thing to expect a high-functioning person whose primary clinical focus is substance abuse treatment to complete a 25-question Telephone Monitoring and Adaption Counseling survey before each meeting with a counselor, but quite another to expect people with unstable housing, low levels of literacy and very limited attention capacity (which is a large part of the target population) to complete that same survey before each meeting. While technology may not work for every client in your program, evidence shows that a very high percentage of participants do have access at least to cell phones and can navigate modest electronic services. The venders you select must be able to deliver solutions that are appropriate to the level of literacy and attention capacity. While these are emerging areas, they do not constitute a barrier to proceed.
In short, the barriers are falling because the potential benefits are just too great.
What kinds of value should we expect?
As shown by early successes, notably Centerstone of Indiana, which has implemented a complete Electronic Recovery Oriented System of Care (e-ROSC) system for substance abuse under the direction of Linda Grove-Paul, VP of Recovery & Innovation Services, value propositions for HIT in addiction services include:
- Improved operating efficiency:
- Using technology to automate many forms of communication that traditionally take a staff person’s time and effort, such as appointment and task reminders and completion. Further, technology can support communication not only between staff and participants but also among participants through social media.
- Better alignment of staff with participant needs. One idea in ROSC is to align staff resources not only with the participant, but also with the need. Qualified peers or bachelor-level staff can meet many clients’ needs for assistance, allowing masters-level and specialized staff to focus on the needs that only they can address. Technology can enhance this alignment of services.
- Improve self-sufficiency by teaching participants to used online tools to find resources or answers that traditionally would require staff assistance.
- Increase the potential for revenue. This is tricky. Since so many participants fall within safety net programs or come from the criminal justice system, and funding policies vary by state, it is hard to generalize about revenue opportunities. The one thing that is clear is that new funding models will start to go into effect over the next two years. Specific funding models include:
- Medicaid Health Homes
- Medicare/Medicaid Shared Savings Program attached to Accountable Care Organizations
- Insurance –based incentive programs
- SBIRT. (While not a big financial opportunity, this is an important source for lead generation.)
- Improved outcomes. None of this means anything if we don’t improve outcomes. Some of the most important outcomes measures include:
- Decreasing the rate of relapse
- Lowering the rate of recidivism
- Decreasing the number of emergency room visits
- Reducing the number of adverse outcomes for pregnant women with substance abuse issues.
- Improved employment patterns, housing, and social stability
Looking at these measures of success, it is clear that a traditional return on investment (ROI) model just doesn’t work. A better model is the net contribution model, based on the accounting theory called Activity Based Costing. Where a traditional ROI model looks purely at the percentage return of one financial investment compared to another, the net contribution model addresses a more broadly defined question “If I invest in this technology and change in work flow, what is the net contribution to my sustainability plan?” This broader approach includes consideration of some of the value statements described above that don’t fit as nicely in a financial ROI model.
Getting the data and running the numbers
One of the biggest challenges in any organization is capturing the data. It is one thing to compare the results of a periodic assessment like Bill White’s Recovery Capital Scale to see the overall effect over time, and even that can be a laborious task. It is quite another to capture and correlate those outcomes measures with an accurate record of interventions. For example, e-ROSC captures accurate data about interventions automatically, thereby simplifying the process of reporting and analyzing the results.
Why is now the time?
There are three reasons why now is the time to adopt HIT:
- ROSC is gaining traction in the industry. Leaders like Centerstone that have gone far to design and implement ROSC based systems, but they are still being refined. That means it’s not adoption of HIT for its own sake. Rather, it is a part of a larger transition in service delivery.
- As we move towards models of integrated care, the business of substance abuse and mental health treatment is itself being re-defined. These newly defined practices can be implemented from the start with HIT built in.
- Here’s the big reason, and there is no gentle way to say this: Where the cost pressures of traditional physical healthcare have forced providers to minimize time spent with patients, behavioral health is focused on effective and timely communication. This means that substance abuse and mental health service providers are ideally positioned to lead this inevitable transition to improved patient engagement.
Next steps.
Just do it. With recent grant opportunities such as the “Grants to Expand Care Coordination through the Use of Technology-Assisted Care in Targeted Areas of Need (TCE-TAC)” from SAMHSA as well as a currently open CMS Innovation grant, funding is available that can absorb the initial cost and reduce the risk. All you have to do is find the right combination of vendors and educate your staff. Your participants are ready and waiting.
Now is indeed the time.
Download PDF Version
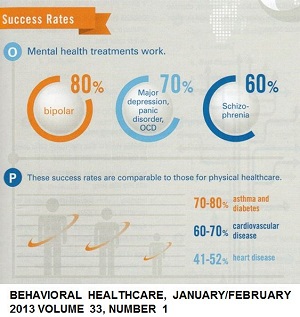 favorably to treatment of asthma & diabetes, cardiovascular disease and heart disease. Advances in neuroscience have increased our understanding of addiction as a brain disease; new treatments are emerging to treat it more effectively. Still, in some states, it is estimated that as few as 10 percent of the people who could benefit from addiction treatment actually receive it.
favorably to treatment of asthma & diabetes, cardiovascular disease and heart disease. Advances in neuroscience have increased our understanding of addiction as a brain disease; new treatments are emerging to treat it more effectively. Still, in some states, it is estimated that as few as 10 percent of the people who could benefit from addiction treatment actually receive it.